We acknowledge and pay respects to the traditional owners of the lands on which MPHN operates; the Wiradjuri, Nari Nari, Wemba Wemba, Perepa Perepa, Yorta Yorta, Ngunnawal, Ngarigo, Bangerang and Yitha Yitha Nations.
We recognise our communities are made up of many Aboriginal and Torres Strait Islander peoples descended from additional mobs and clans who also call the Murrumbidgee region home.
Acknowledging First Nations communities
strategic plan
focus areas
priority areas

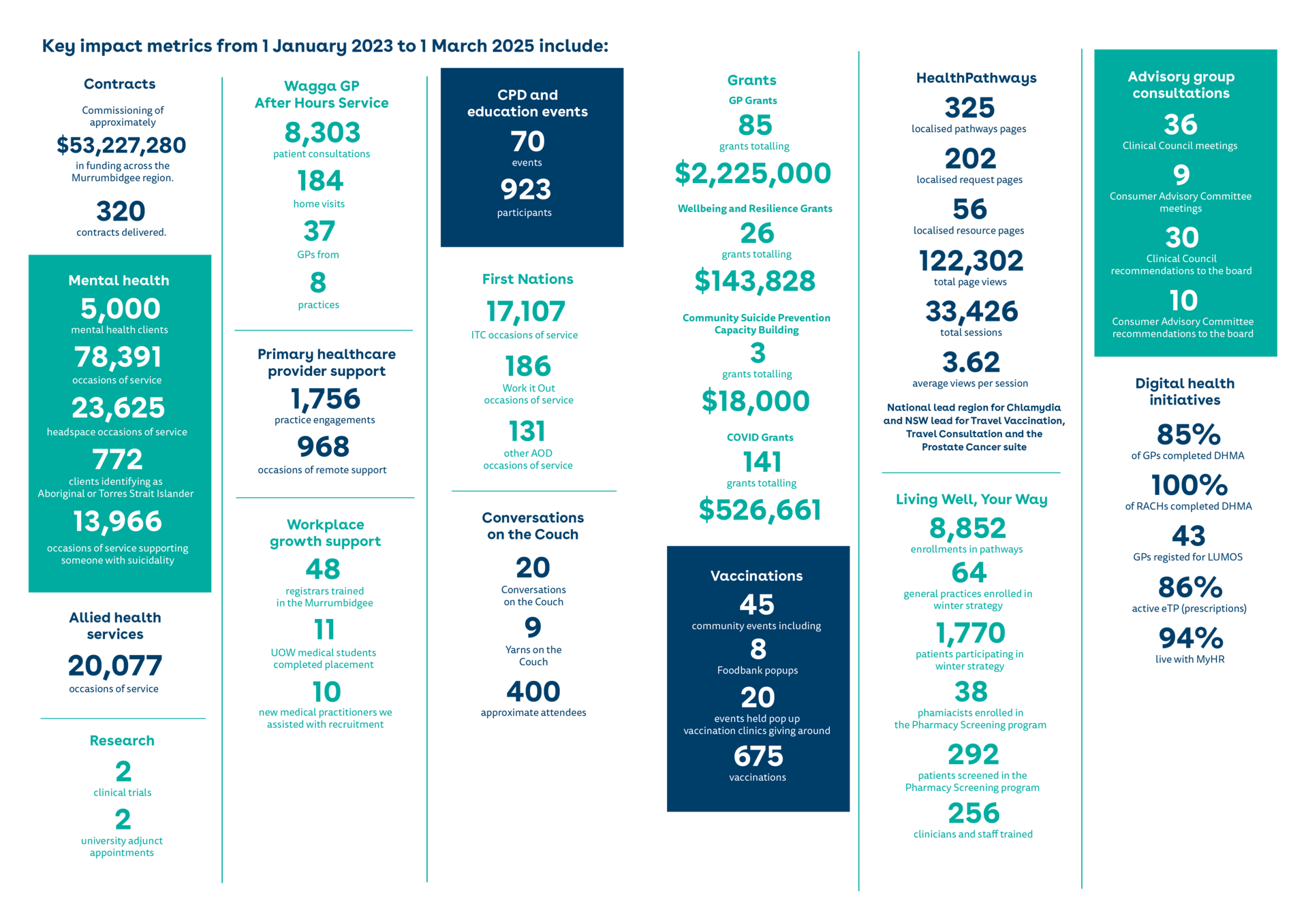
In late 2022, Murrumbidgee Primary Health Network (MPHN) launched its 2023–2027 Strategic Plan, centred around three key focus areas: investing in communities for improved health outcomes, supporting providers and enhancing collaboration for stronger primary healthcare, and leading innovation to inspire positive impact. Twelve priority areas underpin these focus areas, guiding MPHN's efforts toward its vision of well people, resilient communities across the Murrumbidgee. Now at the halfway mark, MPHN has taken the opportunity to reflect on progress and evaluate the impact of its work since January 2023 through to March 2025.
This high-level impact report outlines key achievements, highlights a range of activities aligned to the strategic plan, and includes supporting impact statements, stories, and an achievements gallery. It also maps progress against the three core functions of a PHN: coordinating local health services with hospital networks, commissioning services to address gaps and improve equity, and building capacity within the sector. Despite a rapidly evolving external environment, MPHN and its partners have made significant strides. This report will assist the Board and Executive in understanding these achievements, connecting strategy to operations, and guiding planning for the final two and a half years of the strategic plan.
Sincerely,
Stewart Gordon
CEO
Enablers
MPHN’s impact is underpinned and facilitated by our strategic enablers. These enablers need to be solid and robust to support the organisation.
Stable Board membership and leadership with only one new addition since January 2023.
Board has a number of governance committees that provide oversight and guidance and oversight to the Executive in between Board meetings.
Strong and cohesive executive and senior leadership teams that continues to strengthen.
The organisation actively engages in a robust activity reporting framework including departmental reporting, internal and external auditing activities.
Joint Executive meetings with the Local Health District, key regional stakeholders such as the Health and Knowledge Precinct, development of joint regional planning frameworks to promote a one-health system way of working.
MPHN supports consumer engagement with approximately 300 consumers involved in the Local Health Advisory Committees across the region. These are jointly managed in partnership with the Murrumbidgee Local Health District.
MPHN is an active member of several consortiums, alliances, and collaboratives including Murrumbidgee Mental Health Drug and Alcohol Alliance, Murrumbidgee Aged Care Consortium, Murrumbidgee Aboriginal Health Consortium, and Murrumbidgee Suicide Prevention and Aftercare Collaborative.
In 2024 MPHN hosted a celebratory 30-year anniversary event with more than 100 past and present stakeholders attending or participating in gathering organisation history recording activities
Revenue has increased in the two-year period by 9% to $38 million, with money spent on commissioning services increasing more than revenue at 11% to demonstrate efficiency, and a total of $53.1million spent across 465 contracts.
ISO 9001 Certification was obtained in 2022 and in 2023 and 2024 MPHN obtained a 100% compliance rating.
In 2024 MPHN attended five conferences. Of the 17 conference abstracts submitted, 15 were successful. In 2025, MPHN has been invited to present at three conferences – International Mental Health Conference, International Social Marketing Conference, and Change 2025 Conference.
In 2024 MPHN’s work has been acknowledged with several award accolades including The Mental Health Service Awards, Murrumbidgee Local Health District Excellence Awards, LIFE Award, NSW Public Participation Awards, Pharmaceutical Society of Australia Awards, Rural Health Pro Awards, and the Australian Marketing Institute Awards.
MPHN has 21 employees who have worked at the organisation for five years or more, and 10 who have provided 10 or more years of service.
Commitment to Reconciliation with First Nations peoples through the launch of the organisation’s first Reconciliation Action Plan (RAP) in November 2023, developed by MPHN’s RAP working group.
In the March 2025 MPHN Pulse Survey, 96% of employees would recommend the organisation as a great place to work.
Staff have participated in approximately 300 learning and development activities including attending conferences over the past three years.
Invest in communities for improved health outcomes
Focus area one
Priority area 1.1 – Identify opportunities to design and invest in models of care to improve equity of access, particularly for priority needs and populations.
Improving equity of access is embedded in all MPHN activities including design, commissioning and capability building. Since 2023, MPHN has strived to improve equity of access to primary care across the Murrumbidgee region.
IMPACT: Improving equity of access through responsive service delivery models shaped by community-led co-design and needs assessments.
IMPACT: By partnering with local providers and general practices, it fills service gaps and delivers outreach to improve equity of access.
IMPACT: Improved equity of access to culturally appropriate care for First Nations communities.
IMPACT: Helping rural communities have more equitable access to essential healthcare services, closer to home.
IMPACT: The collaborative model has been in operation for 23 years and is staffed by 37 general practitioners from eight general practices. Since January 2023 the service has provided 11,128 clinic consultations and 241 home visits to residents of residential aged care homes.
MPHN released the LGBTQIA+ Health Needs Assessment, revealing significant challenges faced by the local LGBTQIA+ community when accessing healthcare.
The assessment shows the compounded disadvantage LGBTQIA+ community members experience due to a lack of safe and inclusive healthcare services, with people delaying or avoiding seeking healthcare due to fear of discrimination or judgment.
Report highlights healthcare challenges faced by LGBTQIA+ community
“We need to create a healthcare system that understands and supports everyone. When we look at the concerns people have, like social isolation, financial hurdles, and the importance of better communication and education, it really emphasises the need for specific actions to boost the health and wellbeing of the LGBTQIA+ community in our region.”
Anita McRae, Senior Manager Priority Populations
MPHN was proud to launch a new toolkit designed to help GPs and general practice staff create culturally safe and inclusive environments for First Nations patients.
The Murrumbidgee First Nations Toolkit for General Practice aims to support general practices across the region in addressing the challenges First Nations people face when accessing healthcare through mainstream services.
New toolkit supports GPs in creating culturally safe spaces
“I’m looking forward to working with general practices and offering ongoing guidance as they implement the toolkit and build their cultural competence.”
Maxine Honeysett, Aboriginal Health and Wellbeing Manager
Priority area 1.2 – Work with partners to address the social and cultural determinants of health that are most impacting our communities.
The social and cultural determinants of health have a significant impact on health equity. By collaborating with our partners, MPHN is better positioned to address these factors effectively.
IMPACT: Improved health and wellbeing outcomes for children and families.
IMPACT: These partnerships help embed social and cultural determinants of health into service design, resulting in more inclusive and effective care.
IMPACT: Two Medicare Mental Health Centres have been commissioned in Wagga and Young in 2024 that provide a holistic approach to mental health services and addressing social and cultural determinants of health.
IMPACT: Amplified lived experience voices and improved community-driven mental health and AOD support.
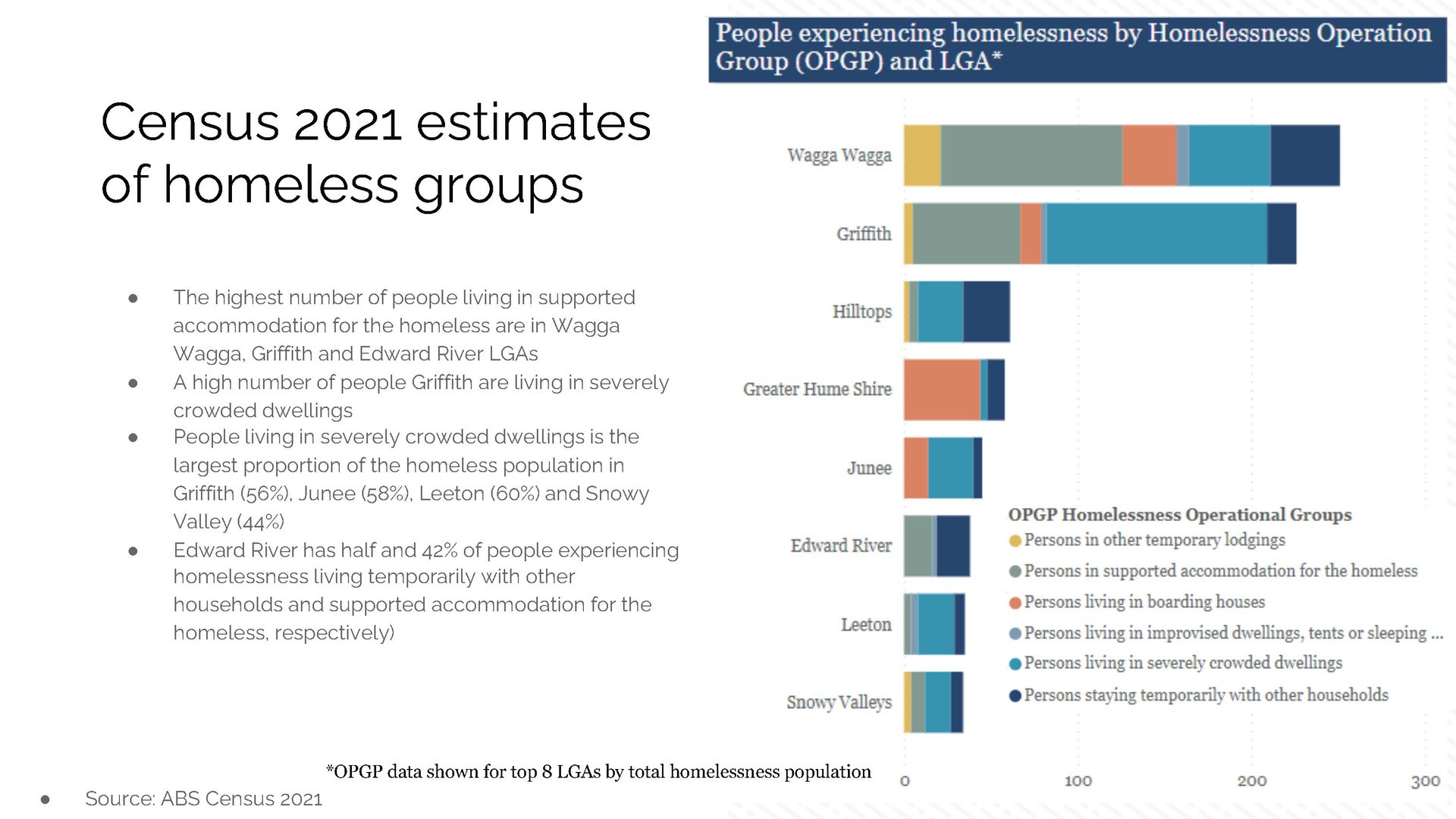
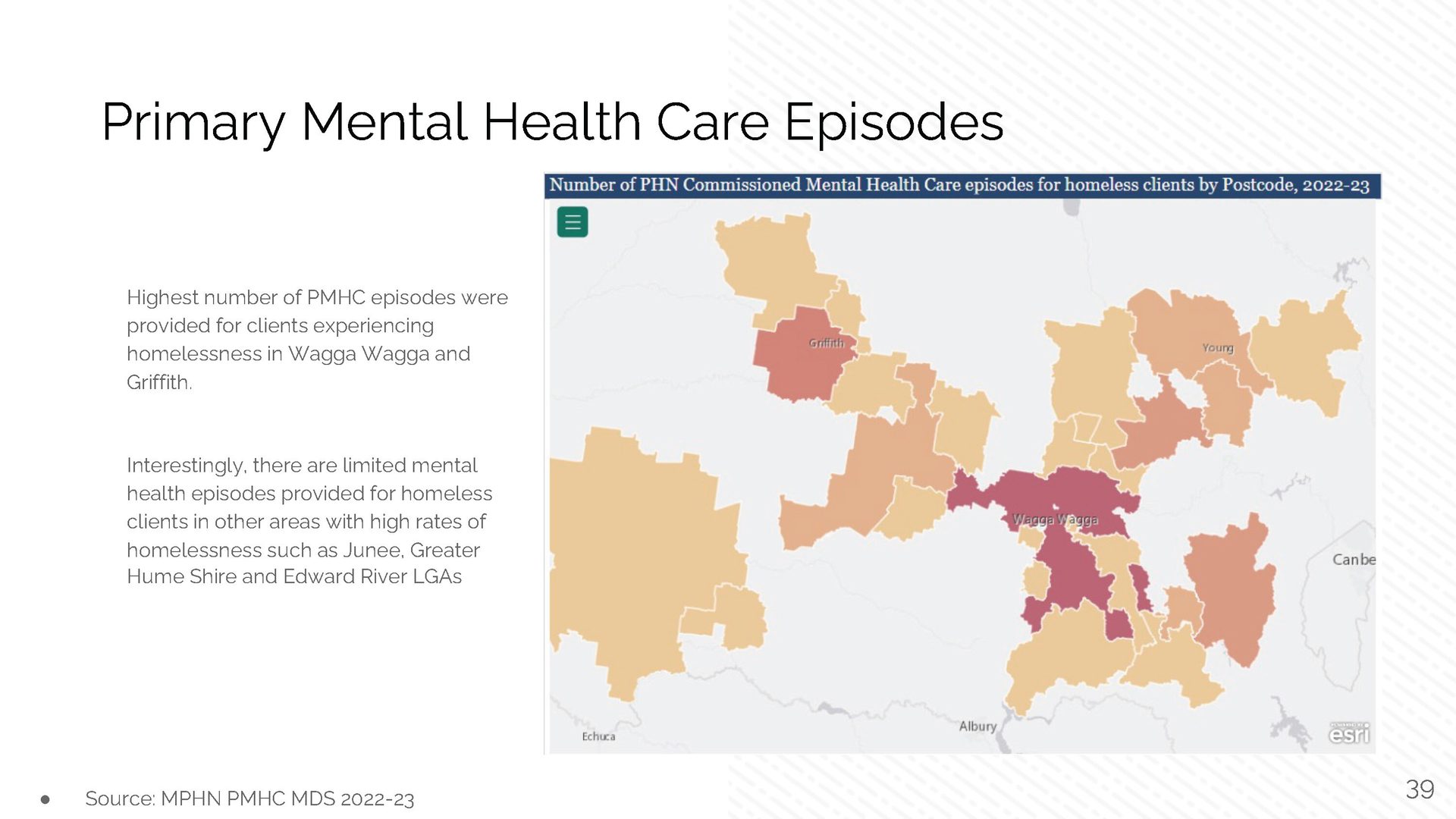
One of MPHN’s key findings over the last few years has been the rise of homelessness and issues with housing affordability and lack of affordable rental properties across the Murrumbidgee.
MPHN commissioned Beacon Strategies to undertake a homelessness-specific Health Needs Assessment (HNA). The HNA involved a stakeholder engagement session with representatives from housing, social and health sectors, with findings triangulated with population health and service utilisation data.
The HNA identified several areas of need including affordable and timely access to primary and specialist care, and opportunities to explore outreach models bringing services to where people are living. MPHN secured department funding to deliver a Homelessness Health Support Program in 2024/25 and is looking forward to delivering this program in the coming year.
Homelessness health support
Priority area 1.3 – Enhance our understanding of consumer experience and outcomes to deliver high value care.
MPHN has enhanced our understanding of consumer experience and outcomes through a variety of mechanisms and programs.
IMPACT: Improved patient care, targeted investments in high-value services, and the ability to refine programs based on patient-reported outcomes for better health experiences.
IMPACT: A more consumer-centred healthcare system, improved service planning through data-driven insights, and stronger stakeholder collaboration to address local health needs.
IMPACT: The network shares expertise with agencies, peak bodies, and government, contributing to MPHN co-design and evaluation.
IMPACT: This collaboration improves consumer experiences and community access to aged care.
IMPACT: This deep community input directly informs the design and delivery of high-value, person-centred care across the region.
MPHN’s Connect, Your Way campaign has been recognised with three awards for its contribution to mental health awareness.
The campaign has won several accolades including Purpose-Led Marketing Award at the 2024 Australian Marketing Institute (AMI) Marketing Excellence Awards, the NSW Public Health Association Communication Award, and Mental Health Promotion or Mental Illness Prevention Award from the Mental Health Services Learning Network. The campaign also reached the finals of the Research Society’s Research Awards in 2023.
MPHN co-designed the Connect, Your Way campaign with more than 60 Murrumbidgee residents who shared their experiences of mental health challenges and accessing support. The campaign was bought to life by five locals who bravely shared their mental health experiences and stories.
Murrumbidgee voices propel mental health campaign to major award wins

“The contributions of local people allowed our team to create a campaign that resonated deeply, not only with the Murrumbidgee community, but obviously with many people, given the campaign’s success. It highlights the importance of listening to and learning from people who have experienced mental health challenges when creating mental health resources. We’re deeply grateful for their input and proud to have developed such a valuable resource.”
Stewart Gordon, Chief Executive Officer
Priority Area 1.4 – Embed practices that support resilience and respond to emerging health and environmental impacts.
MPHN continues to strengthen its work in supporting the resilience of our communities and responding to emerging health and environmental impacts.
IMPACT: Increased community access to vital vaccinations and health checks, improved public health protection, and enhanced food security for over 6,000 people through MPHN-sponsored Foodbank pop-up clinics.
IMPACT: Nearly half of the region’s general practices are using the Emergency Response Planning Tool to maintain care continuity during disasters.
IMPACT: This funding helped communities recover from disasters while strengthening local partnerships.
IMPACT: This collaboration strengthens regional coordination and improves emergency response efforts across the Murrumbidgee.
IMPACT: By maintaining strong relationships with local practices and engaging through Local Health Advisory Committees, MPHN helps reduce the impact on affected communities.
MPHN has travelled across the Murrumbidgee engaging with communities, providing free vaccinations and sharing vital health information with people in need.
A significant focus of our community engagement has been ensuring access to immunisations. Throughout the year, we organised multiple pop-up vaccination clinics which delivered a range of free vaccines, including COVID-19, influenza, and Japanese encephalitis (JE).
Events like the Henty Machinery Field Days, Big Picnic, and Junee International Women’s Day Expo allowed MPHN to connect with the community.
In December 2023, MPHN sponsored a Foodbank pop-up event in Wagga Wagga, which provided crucial food relief ahead of the holiday season, distributing eight tonnes of fresh produce to hundreds of families. Free health checks were also offered at the event.
MPHN has attended 45 community events including eight Foodbanks, giving approximately 675 vaccinations to hard-to-reach populations.
Out and about in the community
“Meeting with people in their own communities helps us understand their unique needs, connect them with health service information, and offer free vaccinations to those who may be vulnerable or have fallen behind with their healthcare. It’s also a great environment to chat about mental health and get people connected with relevant healthcare providers. Having these relaxed conversations helps us foster a healthier and more informed community.”
Peta Anderson, Clinical Programs and Emergency Response Manager

Support providers and enhance collaboration for stronger primary healthcare
Focus area two
Priority area 2.1 - Partner with general practice and primary health providers to support the wellbeing and sustainability of the workforce.
A core focus of MPHN is supporting the wellbeing and sustainability of the primary care workforce across the region. This work has been intensive and impactful, delivered through a variety of initiatives.
IMPACT: This strong connection drives quality improvement and supports innovations like the DREAM diabetes outreach clinics.
IMPACT: These initiatives strengthen workforce capability, connection, and overall retention.
IMPACT: The program has engaged over 30 GPs, strengthening collaboration, connection, and shaping locally tailored support.
IMPACT: Their input helps guide registrar distribution by reviewing data, providing insights, and engaging with stakeholders.
IMPACT: These collaborations help build strong training pathways, increase workforce visibility, and drive long-term sustainability.
IMPACT: These grants have enhanced practice infrastructure, supporting improved service delivery and patient care.
in person general practice visits annually
MPHN undertakes approximately
GP registrars annually in the Murrumbidgee
MPHN supports training of approximately
new practitioners annually into the Murrumbidgee region
MPHN supports the recruitment and onboarding of approximately
new practitioners annually into the Murrumbidgee region
MPHN assisted approximately
In an effort to provide more face-to-face engagement opportunities with our busy GPs, MPHN has launched a new initiative, The Doctors Table, to bring doctors together for dinner and conversation.
Firsthealth Board Chair Dr Jodi Culbert said the initiative aims to provide the opportunity for general practitioners to relax after work with colleagues and to discuss the issues and opportunities in the region.
Introducing The Doctors Table
“It is so important to take some time to recharge and be energised by discussing ideas and opportunities to address the various issues and challenges we face in practice.”
Dr Jodi Culbert, Board Chair
MPHN invited general practices across the region to apply for funding through the Strengthening Medicare – General Practice (GP) Grants Program, part of a $220 million national investment by the Department of Health and Aged Care. The initiative complements MPHN’s broader efforts to support local implementation of national healthcare reforms like MyMedicare and increased bulk-billing incentives.
Eighteen general practices across the region shared in $460,000 in grant funding. Tumbarumba Medical Practice, for example, used its $25,000 grant to enhance its digital capability and infection control, purchasing a defibrillator, upgrading the vaccine fridge and server, and installing HEPA-filtered air conditioning.
Helping implement primary healthcare reform locally

Priority Area 2.2 – Continue building the capacity and capability of local general practice and broader primary health services and support them to lead primary care reform locally.
MPHN has worked locally to build the capacity and capacity of local services to lead primary care reform.
IMPACT: With approximately 30-40 clinical representatives at any time, their input ensures that local issues and reform implications are considered, leading to more responsive, effective, and community-focused healthcare solutions.
IMPACT: By integrating allied health perspectives into planning and strategy, MPHN is enhancing service delivery, improving patient outcomes, and addressing workforce challenges.
IMPACT: Policies and decisions are more reflective of local healthcare needs, leading to more effective and relevant health outcomes for the community.
The Enhanced Paediatrics in Primary Care (EPiPC) program is making a significant difference in the lives of young children across the Murrumbidgee region by providing early intervention for behavioural and developmental issues through a coordinated, community-based approach.
Since commencement EPiPC has continued to aid children and their families across the Deniliquin, Gundagai, Hay, Wagga Wagga, and Leeton communities. GPs continued to enhance their professional development, conduct screenings, and provide extended appointments for children with behavioural and developmental concerns.
Recent success stories include instances where children were supported without needing in-person paediatric appointments. Through email consultations, GPs received community paediatrician advice, enabling timely support and reducing wait times.
Another initiative making a difference is WARATAH for Kids, which is helping young children facing developmental delays by facilitating assessments and referrals to allied health services.
Over the course of 42 clinics, 109 children were seen, receiving timely assessments and support.
One success story is that of 7-year-old Ollie*, who was struggling with sensory processing, emotional regulation, and behavioural issues. Through WARATAH for Kids, Ollie was referred to an occupational therapist (OT) for a comprehensive intake and assessment. With the OT’s guidance, Ollie’s family received tailored strategies and referrals, ensuring timely and coordinated care that allowed Ollie to thrive.
* Name changed
Enhancing paediatric care for a brighter future
“The collaboration between our GPs, paediatricians, and allied health teams ensures families can access the right care when they need it. This program is helping communities to build stronger foundations for the future health of their children, and we’re really pleased with the positive impact it’s having across the Murrumbidgee.”
Christina Eastall, Contracts Manager

Allied health professionals are integral to primary healthcare, and are essential for improving access, outcomes, integration, safety, and quality across the health system.
In 2023, the National PHN Cooperative launched the National PHN Allied Health in Primary Care Engagement Framework to enhance engagement between Primary Health Networks (PHN) and the allied health sector. This framework will guide MPHN in strengthening collaboration and support with allied health practitioners in the region.
In May 2024, MPHN held focus groups with allied health clinicians to identify key challenges and opportunities. Feedback highlighted workforce shortages, the need for stronger collaboration with general practice, improved digital health integration, business support, networking, and allied health-specific CPD events. In response, MPHN launched a dedicated allied health web page and established an Allied Health Advisory Group.
Fostering allies in health

Priority area 2.3 – Enhance collaboration with new and existing partners to enable integrated responses to health needs.
MPHN has enhanced collaboration to improve integrated care across multiple activities from 2023 to 2025. Below are just a few examples of these efforts and their impacts.
IMPACT: Its 15 initiatives have delivered profound community impact, positioning MPHN as a national leader in collaborative commissioning.
IMPACT: These efforts enhance sector knowledge, foster connection, and improve care transitions for older people across the region.
IMPACT: These partnerships ensure MPHN stays connected, influential, and well-positioned to lead meaningful local change.
IMPACT: Improved integration of healthcare services and more strategic, region-specific planning that enhances the overall effectiveness and accessibility of care for the community.
The Living Well, Your Way (LWYW) initiative is transforming how care is delivered for people with chronic conditions in the Murrumbidgee region, focusing on innovative, patient-centred solutions that improve access to affordable and equitable healthcare. A collaboration between MPHN and Murrumbidgee Local Health District (MLHD), funded by NSW Health, LWYW was co-designed with over 200 local stakeholders to address regional needs and improve care for people living with Chronic Obstructive Pulmonary Disease (COPD) and Congestive Heart Failure (CHF). By working closely with local healthcare professionals, the initiative tackles challenges like long travel distances and high healthcare costs, with a particular focus on reducing preventable hospitalisations.
LWYW includes a range of programs, such as pharmacy screening, outreach diagnostics, expanded primary care services, and culturally appropriate rehabilitation. Key components include the Outreach Heart Failure Diagnostic Clinic—a public-private partnership that improves heart failure management—and outpatient clinics in Wagga Wagga for respiratory and heart failure care. The initiative also launched a culturally safe rehab pilot for Aboriginal and Torres Strait Islander communities, trained local physiotherapists to deliver Lungs in Action classes, expanded Wagga Wagga Base Hospital’s Rapid Access Clinic to ease ED pressure, and introduced the CareMonitor app to help patients track their health at home.
One health system mindset - Living Well, Your Way program
“Working together with local health professionals and community members is essential in helping people with chronic conditions live well. By combining our strengths and resources, we’re not just improving individual health outcomes, we’re fostering a supportive and better-connected community.”
Caroline Holtby, Director Collaborative Commissioning
“This Collaborative Agreement formalises the existing partnership and strong commitment between both organisations to work towards a shared vision of one health system for the Murrumbidgee.”
Glynis Ingram, MLHD Board Chair
MPHN and MLHD have formally committed to improving the health and wellbeing of Murrumbidgee communities by strengthening their partnership and collaborative efforts. In late 2022, the boards of MLHD and firsthealth Limited came together to discuss challenges and future opportunities, resulting in a formal Collaborative Agreement. MPHN’s firsthealth Board Chair, Dr Jodi Culbert, highlighted the ongoing challenges faced in regional and rural healthcare, noting that both organisations remain dedicated to implementing NSW and federal healthcare reforms, while also advocating for local change when needed. She emphasised that this partnership has evolved into a mature and advanced model, ensuring access to quality, coordinated healthcare regardless of location.
MLHD Board Chair, Glynis Ingram, echoed the importance of this partnership, stating that collaboration is key to successfully delivering government reforms and initiatives. She stressed that the unique relationship between MLHD and MPHN is vital in supporting both healthcare providers and the communities they serve. By working together, the organisations aim to reduce system fragmentation, enhance sustainability, and streamline healthcare journeys—ultimately improving health outcomes for people across the region.
Joint commitment to one health system approach


Priority area 2.4 – Advocate for communities and primary care providers to influence policy to ensure that local needs are understood and met.
MPHN continues to advocate for and amplify the voices of local communities and primary care providers at both the Commonwealth and state levels.
IMPACT: This advocacy ensures the region’s challenges are recognised by decision-makers, driving more informed and equitable health policy.
IMPACT: This involvement ensures local needs and perspectives inform policies and programs at a broader system level.
IMPACT: These connections support effective advocacy and create opportunities to advance regional health priorities.
As a health leader, MPHN plays an active role in advocating for the needs of its communities and health professionals, with advocacy being a key focus of its Strategic Plan. MPHN has long raised awareness of regional challenges such as workforce shortages, after hours care, and funding. In March 2023, MPHN appeared before the Special Commission of Inquiry into Healthcare Funding in Wagga Wagga to showcase the impact of its collaborative work and to highlight opportunities to strengthen service delivery and care coordination. MPHN also made a submission to the federal Department of Health and Aged Care's review of after hours primary care, shaped by local feedback, and discussed these issues directly with Assistant Minister for Rural and Regional Health, The Hon. Emma McBride MP, during her 2023 visit to Wagga Wagga.
During the Minister’s visit, MPHN showcased local innovations such as the outreach diagnostic heart failure clinics and the Enhancing Paediatrics in Primary Care program, while also facilitating conversations between the Minister and local GPs about the challenges surrounding Strengthening Medicare reforms. MPHN further contributed to the National PHN CEO Cooperative’s submission to the Australian National Audit Office’s audit into the Department of Health and Aged Care’s performance management of PHNs. Published in February 2024, the report made eight recommendations around performance, evaluation, and data. Acting CEO Narelle Mills noted that MPHN’s programs are already delivering improved health outcomes, and these could be better supported through enhanced collaboration with the Department.
Advocating for health in the Murrumbidgee
“As an organisation focussed on supporting primary care providers across the region, we have a role in improving coordination of care, commissioning primary care services to meet local population health needs, and supporting capacity building to ensure a sustainable workforce.”
Narelle Mills, Executive Integration and Partnerships

Lead innovation and inspire for positive impact
Focus area three
Priority area 3.1 – Trial, monitor and evaluate innovative approaches that will achieve improvements to primary care.
MPHN implements innovative approaches that will improve the delivery and access of primary care across the region.
IMPACT: This structured approach drives innovation, ensuring impactful and forward-thinking solutions for local health needs.
IMPACT: The insights enabled tailored action plans and boosted uptake of key digital tools, strengthening primary care capability across the region.
IMPACT: This led to improved end-of-life experiences for residents and families, reducing unnecessary hospital transfers.
IMPACT: These tailored local solutions transform national programs into community-focused strategies that enhance patient outcomes.
IMPACT: Initiatives like pharmacy-based COPD screening have improved outcomes and broadened access to care across the region.
IMPACT: New approaches are strategically designed and effectively implemented for lasting impact.
For many rural Australian communities, pharmacists are trusted and accessible primary healthcare professionals, with patients often visiting their pharmacy for symptom management before their doctor. It makes pharmacists uniquely positioned to identify patients presenting with early symptoms of chronic disease.
As part of the Living Well, Your Way program the COPD and CHF Pharmacy Screening Pilot identifies at risk patients and links them with their general practitioner (GP) for assessment and diagnosis to improve health outcomes and reduce the rate of hospitalisations.
Living Well, Your Way Community Pharmacist Kym Ramsey said the feedback from his peers has been inspiring. However, patient stories demonstrate the real value in the program.
Key to the pilot’s success was involving GPs and pharmacists to codesign screening tools, workflow, and referral processes.
“On presentation to a pharmacy, patients identified as potentially at risk are invited to be screened. Screening utilises a codesigned questionnaire and may include micro spirometry for COPD. Those shown to be at increased risk are referred to their nominated GP for further assessment and possible early diagnosis, improving their long-term health outcomes,” Mr Ramsey explains.
It’s an exciting time for the Living Well, Your Way program and MPHN is keen to see how innovative programs like pharmacy screening can contribute more broadly to the Australian healthcare system.
Rural pharmacy screening for chronic disease
“A 79-year-old woman who previously smoked and presented to the pharmacy with shortness of breath, swollen ankles/feet and fatigue was identified by the pharmacist for COPD and CHF screening. The results triggered a GP referral who referred her to a respiratory physician for further assessment. Through this early intervention she is more likely to manage her symptoms at home and reduces her risk of hospitalisation and further complications.”
Kym Ramsey, Living Well, Your Way Community Pharmacist


Priority area 3.2 – Build collaborative research partnerships that build evidence and contribute to improving the health of local communities.
MPHN has made great inroads into forming collaborative research partnerships and strengthening research capabilities and capacity.
IMPACT: Sharing the strategy with Sector Clinical Councils has boosted clinician awareness and engagement in regional research efforts.
IMPACT: These positions enhance research capacity through collaboration, access to expertise, and valuable university resources.
IMPACT: Local co-design workshops, professional development events, and sector engagement ensure Murrumbidgee’s primary care workforce benefits from and contributes to world-class research.
IMPACT: This partnership strengthens university collaboration and ensures primary care remains central to the research.
MPHN and Wagga Wagga Base Hospital (WWBH) have partnered to deliver the ASPIRE trial in our region with the aim of reducing medication-related harm at transitions of care.
The transition of care from hospital to home is widely recognised as a period of increased risk for medication-related harm. Older people or those taking high-risk or multiple medications are typically more vulnerable.
The ASPIRE Trial is a multi-centre study, sponsored by the University of Sydney, which investigates a PHN-based model of arranging timely medication reviews for people at high risk of medication-related harm when transitioning from hospital to home. Murrumbidgee is one of four trial sites across New South Wales and Queensland.
The trial, scheduled to run until 2025, will evaluate the implementation of a health service interventional program which aims to enhance both the uptake and the effectiveness of Home Medicines Reviews for people post hospital stay. This targeted intervention aims to reduce unplanned hospital readmissions, improve quality of life and reduce medicines burden.
ASPIRE Trial: A systems approach to enhancing community-based medication review

Priority area 3.3 – Empowering clinical and community leaders to influence change in primary healthcare.
MPHN has empowered local leaders to influence change through a variety of mechanisms across the primary healthcare sector.
IMPACT: The panel will build the capacity and confidence of local clinicians to lead reform across a broad range of primary healthcare areas.
IMPACT: Clinical guidelines are regionally relevant, supporting better decision-making and patient care.
IMPACT: Annual planning and events like the 2023 forum provide vital insights that shape MPHN’s aged care priorities and initiatives.
To support the leadership of MPHN’s four Clinical Councils, each council has successfully led and completed innovative projects in their region to address local health needs. In the west, the Western Clinical Council delivered a Community Diabetes Education Program (CDEP) targeting culturally and linguistically diverse (CALD) populations, with a focus on Italian and Pacific Islander communities. The program, developed in response to rising emergency department presentations for diabetes-related complications, was delivered in collaboration with multicultural health workers and community leaders. The initiative provided practical, patient-centred education to help people manage their Type 2 diabetes and reduce hospital presentations.
In Wagga Wagga, two important projects have now been completed. The first established a dedicated clinic to increase uptake of MBS 715 health checks for Aboriginal and Torres Strait Islander children. The second was a pilot of the Students as Lifestyle Activists (SALSA) program at The Rock Central School. This peer-led initiative saw university students train Year 10 students to become lifestyle ambassadors for their younger peers, promoting healthy eating and physical activity.
Meanwhile, the Border Clinical Council completed projects focused on continence care and prostate cancer support. In response to a shortage of continence services in the region, MPHN partnered with the Continence Foundation of Australia and the Rural Doctors Network to train and support practice nurses through online modules, scholarships, and a new community of practice.
The Council also introduced initiatives to improve support for men with prostate cancer, including the rollout of the ‘Bins for Blokes’ campaign in the Snowy Valleys and Wagga Wagga. These targeted projects reflect the valuable insights and leadership of local clinicians in shaping primary care services.
Innovating for impact
“One of the goals of our Strategic Plan is to lead innovation and inspire for positive impact. We engaged with each of the Clinical Councils to understand what local challenges they were facing and how might we be able to support innovative solutions. Its been really exciting to support our Clinical Councils in their projects and looking for innovative solutions for their identified local issues”
Narelle Mills, Executive Integration and Partnerships
Priority area 3.4 – Identify opportunities for new investment into the Murrumbidgee to address unmet needs.
MPHN is intentionally investigating and advocating for new investment into the Murrumbidgee region to address unmet needs.
IMPACT: $3.5 million from competitive funding submissions has enabled targeted applications across priority areas including CALD communities, homelessness, family and domestic violence, aged care in thin markets, and multidisciplinary care models.
IMPACT: Current philanthropic for the DREAM and First Nations Last Days initiatives is helping address service gaps and extend regional impact.
IMPACT: Since July 2023, four proposals have been implemented, driving innovation and delivering targeted care in areas like antenatal health and children’s wellbeing.
Limited access to specialists and allied health services, which are often restricted by availability, cost, and long waitlists, are just some of the common challenges faced by people living with diabetes in the Murrumbidgee region of New South Wales. But thanks to the local implementation of the Diabetes Regional Education, Access, and Management (DREAM) Initiative, these barriers are being addressed.
In 12 months, the Murrumbidgee DREAM initiative has supported 203 people with diabetes through 15 general practice clinics in the rural communities of Tumut, Gundagai, Young, Hay, Adelong, Leeton, Lake Cargelligo, West Wyalong, Griffith, Henty, Finley, Oaklands, and Cootamundra; and 94 health professionals across 15 general practices have participated in one or more professional development sessions.
The program was co-designed with local healthcare providers to ensure the solutions meet the specific needs of communities in the Murrumbidgee and is a result of a collaboration between St Vincent’s Health Network Sydney, St Vincent’s Curran Foundation, MLHD and MPHN.
Murrumbidgee DREAM team – bringing specialist diabetes care to rural NSW
“It really is a dream. Being in the Murrumbidgee is helping us better understand the unique challenges and needs of rural communities in managing diabetes, but equally important is patients having equity of service with their city cousins.”
Gael Holters, St Vincent’s Health Network Sydney Diabetes Clinical Nurse Consultant

KidsXpress was engaged to deliver a whole-class therapeutic program using play and music based therapeutic modalities to encourage the development of healthy peer relationships, support emotional regulation and enhance the emotional wellbeing of children. The program delivered 30 sessions to 49 primary schools students, five teachers and five Student Learning Support Officers with overwhelmingly positive feedback.
Play, music and wellbeing: A therapeutic journey for primary school students
Gallery of achievements







